How do you end a sitcom?
That’s not a joke. For those of us who write sitcoms, it’s a practical question. Every episode needs an ending. These days, every season needs an ending. And then the whole thing needs some kind of grand finale as the characters ride off into the sunset.
A sitcom ending should be both surprising but also retrospectively inevitable. That’s what I tell aspiring sitcom writers. The ending of a sitcom shouldn’t be a nasty shock. Nor is it just the moment where the episode runs out of time or story.
Casablanca is one of the all-time great endings. Rick tells Isla to get on that plane, and there’s the business with Lazlo, Strasser and ‘the usual suspects’. I’ve read that the writing of the ending came fairly late in the day. The Motion Picture Production Code forbade showing a woman leaving her husband for another man. This seems restrictive but in our hearts we want to believe that Rick would do the decent thing.
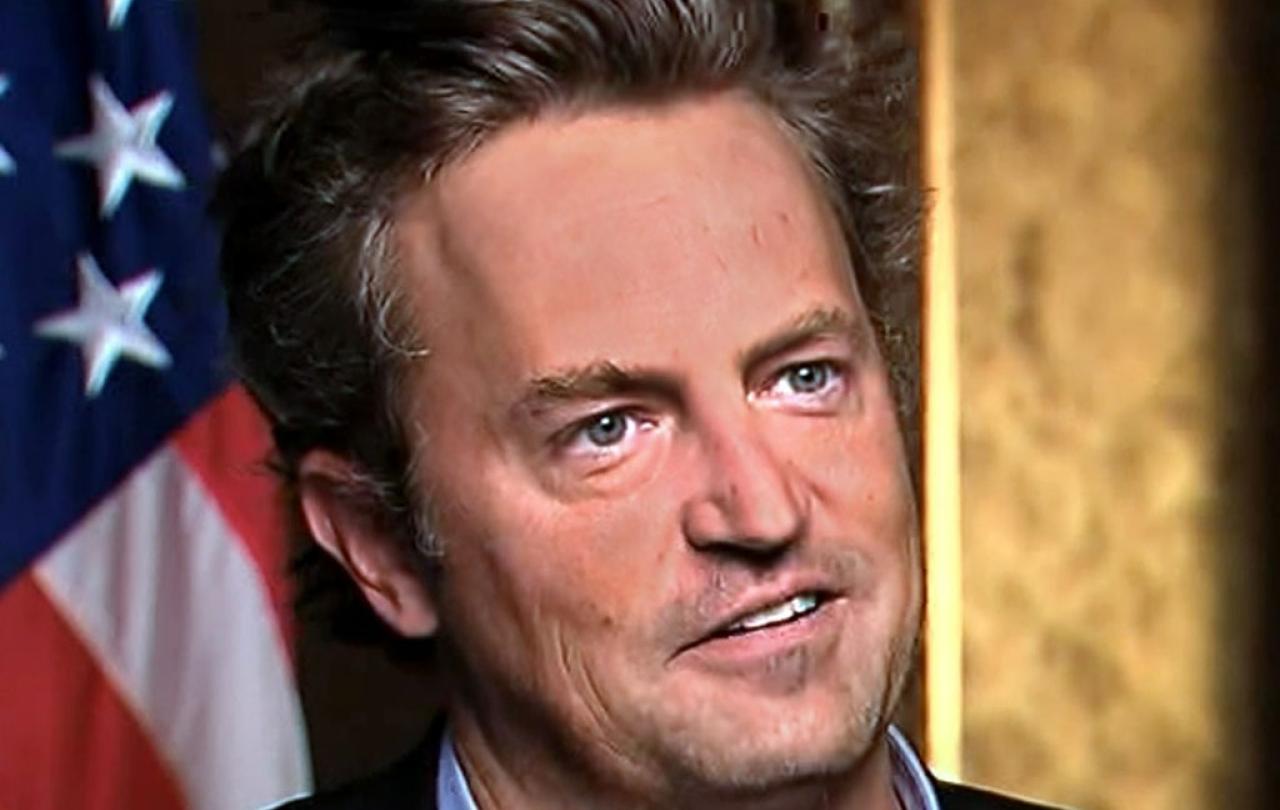
From the very first scene of the very first episode, it was clear that the planets had aligned for this actor, this show and the viewing public. Everybody loved Chandler.
When it comes down to it, our hearts yearn for a happy ending. And if not happy, bittersweet. But mostly sweet.
The ending of Matthew Perry, star of one of the greatest sitcoms of all time, is both surprising and inevitable. No one expected him to die at the age of 54. But given his problems with addiction, it is not as shocking as it might be.
Perry confessed one of his greatest addictions, along with painkillers and alcohol, was to be the funniest. He needed to hear those laughs. In the HBO Max Friends reunion special, he said “To me, I felt like I was going to die if they didn't laugh,” he said. All comedians feel this but it seems that Perry felt it especially acutely. When co-star Matt LeBlanc recalled tripping over his mark and everyone on set laughed, Perry had to jump in. “Because I was like, ‘Somebody's getting a laugh, I can't handle it — I need to get a laugh, too.’”
No wonder Matthew Perry was so funny as Chandler Bing. He was so determined to be the funniest. And he was. From the very first scene of the very first episode, it was clear that the planets had aligned for this actor, this show and the viewing public. Everybody loved Chandler.
For most people, the death of Matthew Perry was the death of Chandler Bing. And we just weren’t prepared for that.
It was a dream character to play: a young man in his twenties who is funny because, well, he is really funny. Being funny is his thing. It’s to cover his cowardice, but he is the funny guy. Ross is the nerd. Joey is the ladies' man. Rachel is the princess. Phoebe is cooky. Monica is uptight. And Chander is the comedian whose lines were being written, rewritten and perfected by a battery of writers who are among the funniest people in the English-speaking world.
But Perry still had to deliver those lines, on cue in the right order, no matter what else was going on in his life. And a lot was going on. But he coped. He was just so funny. The only evidence of his personal demons on screen was his weight loss and weight gain. He was a consistently excellent performer. In an earlier era, when more mainstream romantic comedy movies were made, Perry might have given Cary Grant a run for his money. And then maybe Alfred Hitchcock may have given him a new lease of life.
But I don’t think Perry has been so mourned because of his talent, and that he was taken from us before his time. He wasn’t a River Phoenix or a Heath Ledger whose death meant we have been denied some truly great films they would surely have made. (Personally I feel that way about Victoria Wood who died aged 62 and had at least two more truly great works in her).
For most people, the death of Matthew Perry was the death of Chandler Bing. And we just weren’t prepared for that.
Life isn’t scripted. At least not by us. Sitcoms resemble real life. But our lives are messier, and more complicated. Our jokes aren’t as funny. And sometimes it’s just tragic.
Matthew Perry simply was Chandler from Friends. “I’ve said this for a long time: When I die, I don’t want ‘Friends’ to be the first thing that’s mentioned,” he said. It’s not hard to imagine Chandler making a joke out of that. One can also imagine Perry’s character saying, “I always figured I’d die alone. In a hot tub. Whoa, did I just say that out loud?’ And the audience would laugh because in the Friends-world, those writers have handed Chandler a happy ending: a life with Monica and their children, away from Manhattan, but forever connected to their lifelong friends, Ross, Joey, Phoebe and Rachel.
Life isn’t scripted. At least not by us. Sitcoms resemble real life. But our lives are messier, and more complicated. Our jokes aren’t as funny. And sometimes it’s just tragic. The Chandler Bings don’t get the Monicas and the happily ever afters. Sometimes the Chandler Bings die young and alone. And no-one laughs.
But the real human Perry did what one senses the fictional Chandler Bing would not or could not do: turn to God for help. A year before his death, he wrote in his memoir that at his lowest ebb, he experienced God’s presence and love, saying that “for the first time in my life, I felt OK. I felt safe, taken care of. Decades of struggling with God, and wrestling with life, and sadness, all was being washed away, like a river of pain gone into oblivion.”
Maybe it sounds cliched. But for those of us with a Christian faith, what he experienced is not a surprise but a wonderful reality.





