With one billion molecules of oxygen packed into each of your 30 trillion red blood cells, blood is sometimes known as the red river of life. Countless lives have been saved through blood transfusion, but why, throughout history, across continents and cultures, has there been a special interest in the blood of one man crucified 2,000 years ago, believing it alone to have “wonder-working power”?
Whether you are a newborn baby with half a pint of blood, or an adult with nearer nine pints, “what is certain is that you are suffused with the stuff”, writes author Bill Bryson in his book, The Body.
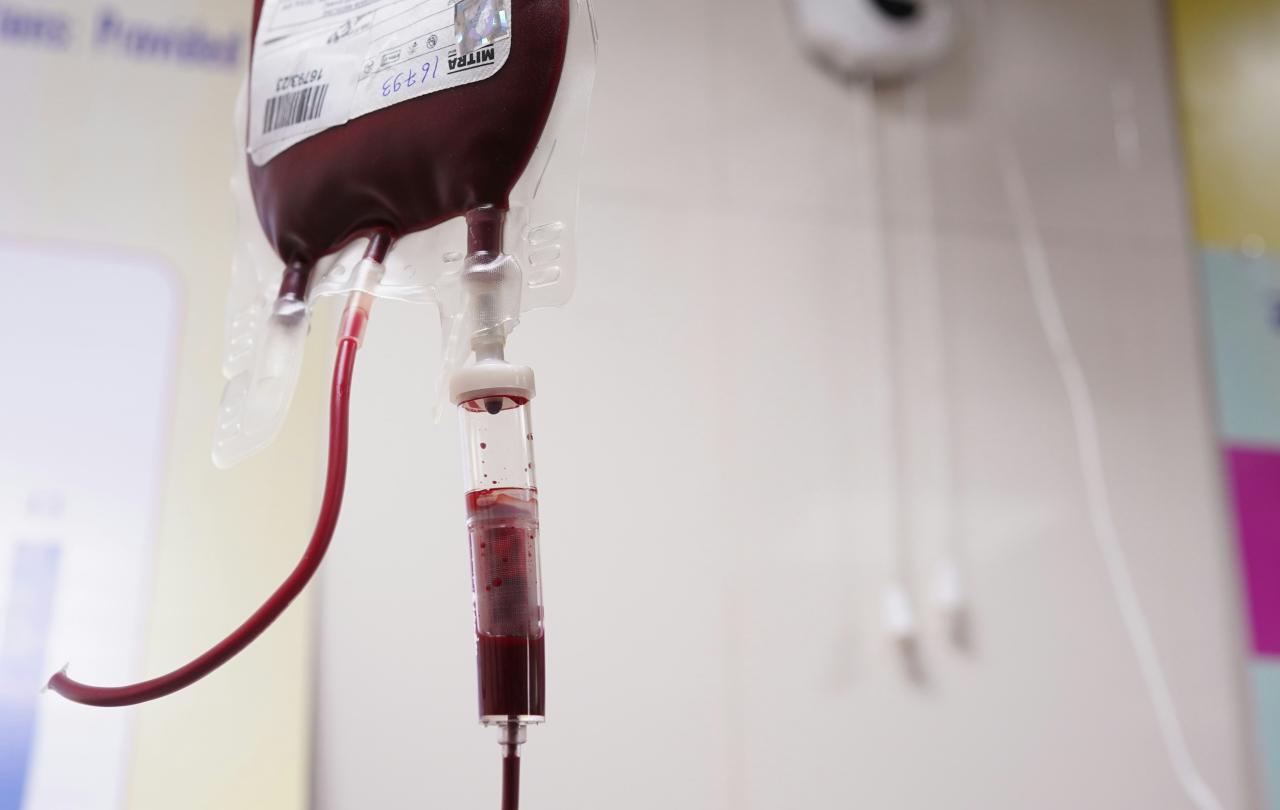
Once thought to ebb and flow in waves like the sea, from the liver to other organs, having been heated in the heart, blood in fact flows in a network of vessels measuring some 60,000 miles, with the heart acting as pump, not heater. Cleverly conserved through a complex system of blood-clotting in the case of injury, blood is a precious resource that needs replacing if lost in large amounts. Victims of road traffic accidents can require up to fifty units of blood; significant amounts are needed for organ transplantation, severe burns or heart surgery.
The first human blood transfusion in Britain, using blood from a lamb, was performed by Dr Richard Lower in 1667, given not to replace blood loss but to change character: could the old be made young, the shy be made sociable through blood transfusion? Apparently not.
Safe transfusion awaited the discovery of blood types by Dr Karl Landsteiner in the early 20th century. Today, NHS Blood and Transplant deliver 1.4 million units of red cells to 260 hospitals each year for transfusion; about 85 million units are transfused worldwide, given to replace blood loss after accident, surgery, ulcer, ectopic pregnancy or for anaemia in cancer. Also used to boost blood cell numbers in malaria, sepsis, HIV, leukaemia and sickle cell anaemia, blood transfusion is now amazingly safe. Fatal reactions are extremely rare, “occurring only in one out of nearly two million transfusions”, writes physician Dr Seth Lotterman. “For comparison, the lifetime odds of dying from a lightning strike are about 1 in 161,000,” he adds. The risk of HIV infection has dropped dramatically, to less than one in seven million.
History tells though of the danger of transmitting disease from the blood donor during transfusion. The World Health Organization recognises risk of infection with HIV, hepatitis, syphilis, malaria, and Chagas disease. The Contaminated Blood Scandal saw an estimated 30,000 people in the UK given blood transfusions and blood products infected with hepatitis C, hepatitis B and HIV. More than 3,000 people died as a result, and thousands more live with on-going health complications. For my final Christmas article for Readers Digest, I wrote on Stephen Christmas, a tireless campaigner for blood safety who lived with haemophilia and died in 1993, having contracted HIV through contaminated blood.
I was a blood donor. However, I am now unable to donate blood or organs for the rest of my life since there is a possibility that my blood is ‘stained’, possibly with prion disease, after adopting embryos. The Blood Transfusion Service will not accept donations from women who have had various fertility treatments.
And there’s another uncomfortable truth about blood donation – the NHS does not have enough blood, organs, tissues, platelets, plasma or stem cells to treat everyone who needs it. As a nurse, I remember caring for a man dying of liver cancer. Suffering from sudden, massive melaena (blood loss in black, tarry stools as a result of internal bleeding), he received emergency blood transfusion, with bag after bag of blood being infused, until the consultant called for the treatment to stop, because the bleed was too big – and blood supplies too scarce.
Struggling to accept the stark reality of stained blood and dangerous shortages, I kept coming back to an old Sunday School song about blood, where absolute abundance and ultimate cleansing are instead promised.
There is a fountain filled with blood
Drawn from Immanuel’s veins;
And sinners, plunged beneath that flood,
Lose all their guilty stains.
Gruesome and graphic in its imagery, but full of deeper meaning. And as a nurse, I’m accustomed to blood, sometimes lots of it. I’ve seen that man bleed out on the ward that night; I’ve attended a road accident, where a boy lost his leg – but not his life, because towels stemmed the massive flow of blood. I’ve raced a patient to the operating theatre after her aortic aneurysm burst within; I’ve stemmed arterial bleeding from the groin by applying prolonged pressure to the site punctured by a catheter during cardiac stenting. According to the World Health Organization, severe bleeding after childbirth is the leading cause of maternal mortality world-wide. Each year, about 14 million women experience postpartum haemorrhage resulting in about 70,000 maternal deaths globally.
In the Bible, and in hymns of praise like this one, there is also no getting away from blood. “Like it or not, the Bible is a bloody book,” writes Kyle Winkler. It runs through the book like a crimson thread. There’s a story of a woman bleeding for twelve years, until she touched the hem of Jesus’ garment and was healed.
Elsewhere the Bible keeps returning to the idea of blood, shed in sacrifice, used to cleanse, save, and heal in a spiritual sense. In the Old Testament, animal blood was painted on doorposts at Passover as a sign of protection from judgment, and sprinkled ritually on the altar as a sacrifice for human sin, restoring relationship with God.
On Good Friday, Jesus himself shed (and sweat) his blood, sacrificing his life on the cross to “wash our souls” once and for all. Millions of Christians across the world take a sip of communion wine each Sunday in commemoration of this act. It’s a beautiful gift, coming with a promise that the shed blood will “preserve thy body and soul unto everlasting life”, through the forgiveness of sins. It’s no wonder then that churches love to sing about this blood. “Would you be free from the burden of sin? There's pow'r in the blood, pow'r in the blood,” goes one hymn, while another simply says, “Your blood has washed away my sin, Jesus, thank you”.
“God’s intention for blood isn’t gory—it’s beautiful! And I’m certainly not offended or scared by it,” writes Kyle. “Rather than question how little blood I can get by with, I’d rather stand under the cross to be covered in all that I can get!” Thank God for the fountain of forgiveness that flows from Good Friday.
Celebrate our 2nd birthday!
Since March 2023, our readers have enjoyed over 1,000 articles. All for free. This is made possible through the generosity of our amazing community of supporters.
If you enjoy Seen & Unseen, would you consider making a gift towards our work?
Do so by joining Behind The Seen. Alongside other benefits, you’ll receive an extra fortnightly email from me sharing my reading and reflections on the ideas that are shaping our times.
Graham Tomlin
Editor-in-Chief





