“What’s that - a face tattoo?”
These were the words of one person as I walked past them on the streets on a recent Wednesday, with the ashes of last year’s burnt palm-branches placed across my forehead in the shape of the cross.
The cross has been a symbol of hope for over two millennia; that even in the most painful of circumstances, darkness does not have the final say, including in death.
As a society, we don’t really talk about death that much. Margot Robbie’s Barbie was the quintessential party-pooper when she pondered:
“do you guys ever think about dying?”.
It’s no fun to dwell on death and dying, and for many of us, we put it off as long as we can. That all changed last year with the introduction of the assisted dying bill into the Houses of Parliament. Our national attention was, for a rare moment, captured by death.
As a parish priest, I’ve seen the finality of burying someone into the ground. I’ve seen the sadness in the eyes of those trying to grieve.
The words of Ash Wednesday, which remind us that we are ‘but dust, and to dust we shall return’ are echoed in the famous words that the priest recites in those last moments of burial, ‘ashes to ashes, dust to dust’. In that moment, amongst the bereaved, there is no escaping the inevitability of death. It is the ultimate statistic, 1 in 1 die.
Whilst death is of course universal and will affect us all, the impact of this assisted dying bill could have consequences for some of the most vulnerable in society.
As I reflect on my time as a Priest in East London, this is not abstract theory, but something I lived with each day. I served amongst a hugely diverse, vibrant, community in one of the poorest parts of the city. As I try to picture some the people I’ve walked alongside, I know it is these lives that will be most affected.
One of the reasons I have concerns about the bill is the prospect of these people being coerced into ending their own lives prematurely, by a world that has already told them their lives are of little value. There are already huge disparities in access to the current provision of palliative care at the end of life, particularly amongst people of colour, the disabled and the poor.
Of the 500,000 people who die each year, 100,000 do not access the care they need. This number is skewed towards ethnic minorities and those who come from poorer backgrounds.
There is much confusion and misinformation about what end-of-life care even is. Research conducted by Marie Curie shows that 1 in 5 people from an ethnic minority background believe Palliative Care is actually Euthanasia.
We only need to look at what has happened around the world when the ‘right to die’ becomes a duty to die. Even with the best of intentions, other jurisdictions show us that safeguards rapidly deteriorate and those who are already vulnerable become even more so.
I worry that the way in which this bill is being handled - rushed through, little time being given to properly chew over the profound consequences it may have - reflects the wider way we view death.
By trying to provide a ‘choice’ for a certain group of people, the consequence will be taking away real choice from those who already have little.
Yet we know that for those who do access it, palliative care can be hugely effective in improving their quality of life, and for some, they can even outlive their prognosis. During Ash Wednesday’s service, I met an elderly gentleman who was diagnosed with stage four pancreatic cancer in 2019. He was told he had five months to live. He described every day of his six-year survival since as a ‘miracle’, his eyes filled with evident joy.
Such a blessing stands in stark contrast to the lonely final days of my 96-year-old great grandmother. She was suddenly taken ill during the Covid-19 pandemic and was frantically rushed to a hospital. Amidst the chaos, exasperated by the restrictions against seeing family that were in place at the time, I distinctly remember confused conversations about placing her in a care home for her final days. It was clear she needed a lot of specialist attention, more than our family could provide ourselves. As she was discharged to stay with our aunt, she never did reach that care home, as she died at home. She was buried in our local cemetery, with our family watching on Zoom.
My final memory of my great-grandmother will be the FaceTime call we shared when she was taken to hospital, with the poor data connection and shaky picture. I am so grateful for the few family members who were able to be by her side when she died, but I’ve often wondered whether she fully received the care she actually needed during those final days, in the way she needed it.
What my great-grandmother didn’t have a lot of at the end of her life was time.
That’s also true for this bill. Concerns have been raised that only five hours of debate were given to this Bill in the chamber, comparatively short for a change in the law of this magnitude.
I worry that the way in which this bill is being handled- rushed through, little time being given to properly chew over the profound consequences it may have- reflects the wider way we view death.
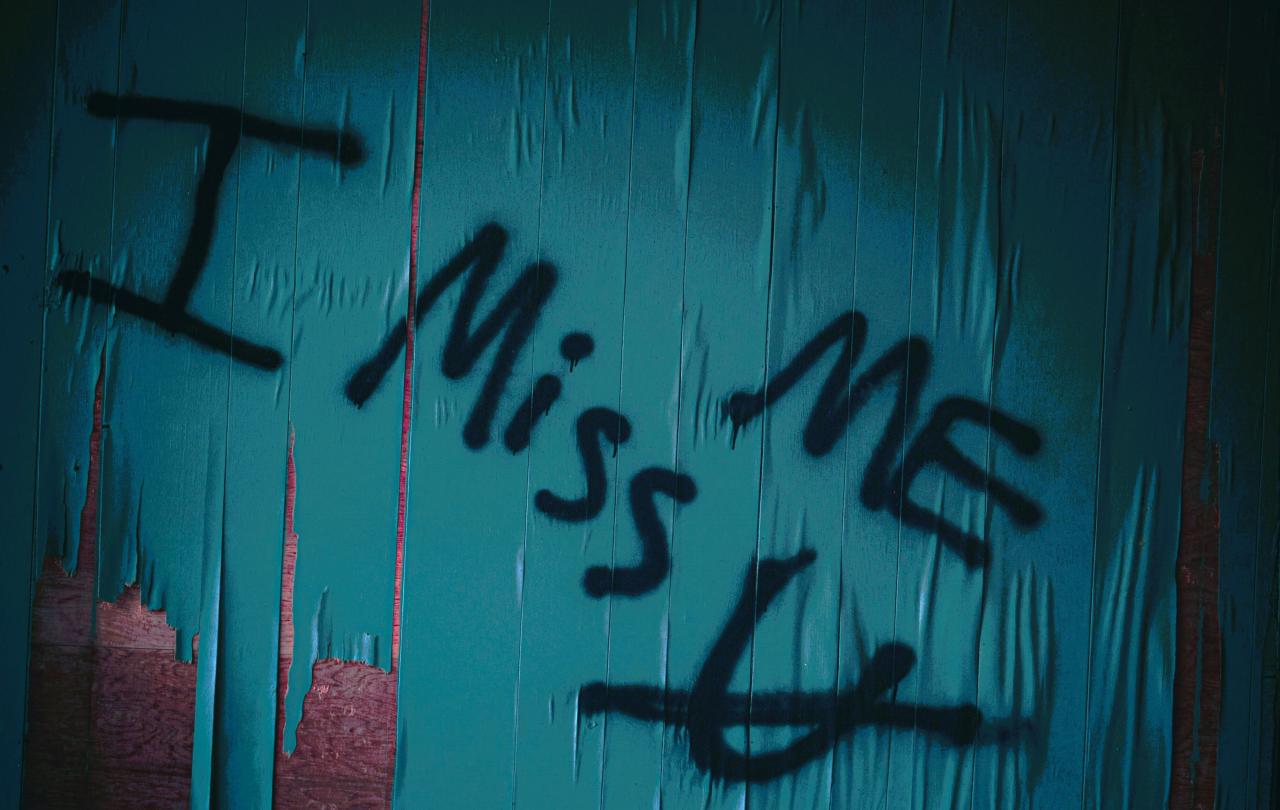
Do we view death - and indeed the dying- as something to be shoved to one side, not spoken about in the hopes we can avoid its impact? Or do we view death as an important moment to review who and what matters most in life?
Perhaps for some, the fact that Christians devote a period of 40 days to dwell on death may be one of the mysteries of faith. However, perhaps it’s not such a bad idea after all. Death may bring with it fear, grief and pain and so we tend to avoid it. But do we risk missing out on much more? As we head into Easter, the cross still serves as a powerful reminder that, especially in death, Hope can be found, that Good has triumphed over evil, and Light shines even in the darkest of places.
Celebrate our 2nd birthday!
Since March 2023, our readers have enjoyed over 1,000 articles. All for free. This is made possible through the generosity of our amazing community of supporters.
If you enjoy Seen & Unseen, would you consider making a gift towards our work?
Do so by joining Behind The Seen. Alongside other benefits, you’ll receive an extra fortnightly email from me sharing my reading and reflections on the ideas that are shaping our times.
Graham Tomlin
Editor-in-Chief